Glaucoma
Glaucoma is a class of eye conditions that can result in blindness and visual loss by harming the optic nerve, which is located at the back of the eye. This damage is often caused by abnormally high pressure in the eye due to an imbalance between the production and drainage of fluid in the eye. Glaucoma is a leading cause of blindness worldwide.
Types of Glaucoma:
There are different types of Glaucoma like Open-angle glaucoma, Angle-closure Glaucoma (Closed-Angle Glaucoma), Normal-tension glaucoma and Secondary glaucoma
Open-angle Glaucoma:
Open-angle glaucoma is the most common form of glaucoma, a group of eye conditions that can damage the optic nerve and lead to vision loss or blindness if left untreated. In open-angle glaucoma, the drainage angle where the iris meets the cornea is open, but the trabecular meshwork, which is responsible for draining aqueous humor (the fluid inside the eye), becomes less efficient over time. This leads to an increase in intraocular pressure (IOP), which can damage the optic nerve and cause vision loss.
Open-angle glaucoma typically progresses slowly and painlessly, often without noticeable symptoms until significant vision loss has occurred. Regular eye examinations are crucial for early detection and management of open-angle glaucoma, as treatment aims to lower IOP to prevent further damage to the optic nerve. Treatment options may include medicated eye drops, oral medications, laser therapy, or surgery, depending on the severity of the condition and individual patient factors. Early detection and treatment are essential for preserving vision and preventing irreversible damage.
Angle-closure Glaucoma:
Angle-closure glaucoma, also known as closed-angle glaucoma or narrow-angle glaucoma, is a type of glaucoma characterized by the narrowing or closure of the drainage angle in the eye. In a healthy eye, there is a small space called the drainage angle between the cornea and the iris, through which the aqueous humor (the fluid that nourishes the eye) flows out. When this angle becomes blocked or narrowed, the aqueous humor cannot drain properly, causing a rapid increase in intraocular pressure (IOP), which can damage the optic nerve and lead to vision loss if left untreated.
Symptoms of angle-closure glaucoma can include severe eye pain, headache, blurred vision, halos around lights, nausea, and vomiting. These symptoms can occur suddenly and are often referred to as an acute angle-closure attack.
Risk factors for angle-closure glaucoma include:
- Age : It is more common in individuals over the age of 40.
- Ethnicity : People of East Asian and Inuit descent are at higher risk.
- Eye anatomy : Hypermetropia (farsightedness) and a shallow anterior chamber increase the risk.
- Family history : Having a family member with angle-closure glaucoma increases the risk.
- Medications : Certain medications, such as anticholinergic drugs, can trigger an acute attack by dilating the pupil and narrowing the drainage angle.
Treatment for angle-closure glaucoma aims to lower intraocular pressure and may involve medications, laser therapy (laser peripheral iridotomy to create a new drainage pathway), or surgery (such as trabeculectomy or goniotomy) to improve drainage. It's important for individuals at risk or with symptoms to seek prompt medical attention to prevent permanent vision loss. Regular eye exams are also essential for early detection and management of glaucoma.
Normal-tension Glaucoma:
Normal-tension glaucoma (NTG), also known as low-tension glaucoma, is a form of glaucoma characterized by damage to the optic nerve and corresponding visual field loss, despite intraocular pressure (IOP) within the statistically normal range (typically defined as less than 21 mmHg).
However, in NTG, optic nerve damage occurs despite normal intraocular pressure. This suggests that factors other than intraocular pressure, such as blood flow to the optic nerve or inherent weakness in the optic nerve, may play a role in the development and progression of the disease.
Symptoms of normal-tension glaucoma are similar to other forms of glaucoma and may include:
- Gradual loss of peripheral vision
- Tunnel vision in advanced stages
- Blurred vision
- Difficulty adjusting to low light conditions
- Halos around lights
- Frequent changes in eyeglass or contact lens prescription
Risk factors for NTG may include a family history of glaucoma, Japanese ancestry, cardiovascular disease, and certain medical conditions such as migraine headaches and Raynaud's disease.
Treatment for NTG typically focuses on lowering intraocular pressure through medications such as eye drops, laser therapy, or surgical procedures. Additionally, regular eye exams and monitoring of optic nerve damage and visual field loss are important for managing the condition and preventing further vision loss. Early detection and treatment are crucial in preserving vision and preventing blindness associated with NTG.
Secondary glaucoma:
Secondary glaucoma refers to a type of glaucoma that occurs as a result of another eye condition or underlying health problem. Unlike primary glaucoma, which occurs without any obvious underlying cause, secondary glaucoma can be linked to various factors such as:
- Trauma : Eye injuries can lead to the development of secondary glaucoma. Trauma may cause damage to the eye's drainage system, resulting in increased intraocular pressure (IOP) and glaucoma.
- Inflammation : Conditions such as uveitis or iritis, which involve inflammation within the eye, can sometimes lead to secondary glaucoma. Inflammatory processes may affect the drainage pathways of the eye, leading to elevated IOP.
- Tumors : Intraocular tumors or tumors pressing on the eye from outside can interfere with the normal drainage of fluid from the eye, causing increased IOP and secondary glaucoma.
- Steroid-induced : Long-term use of corticosteroid medications, whether in the form of eye drops, pills, or injections, can increase the risk of developing secondary glaucoma. Steroids can cause an increase in eye pressure by affecting the eye's fluid dynamics.
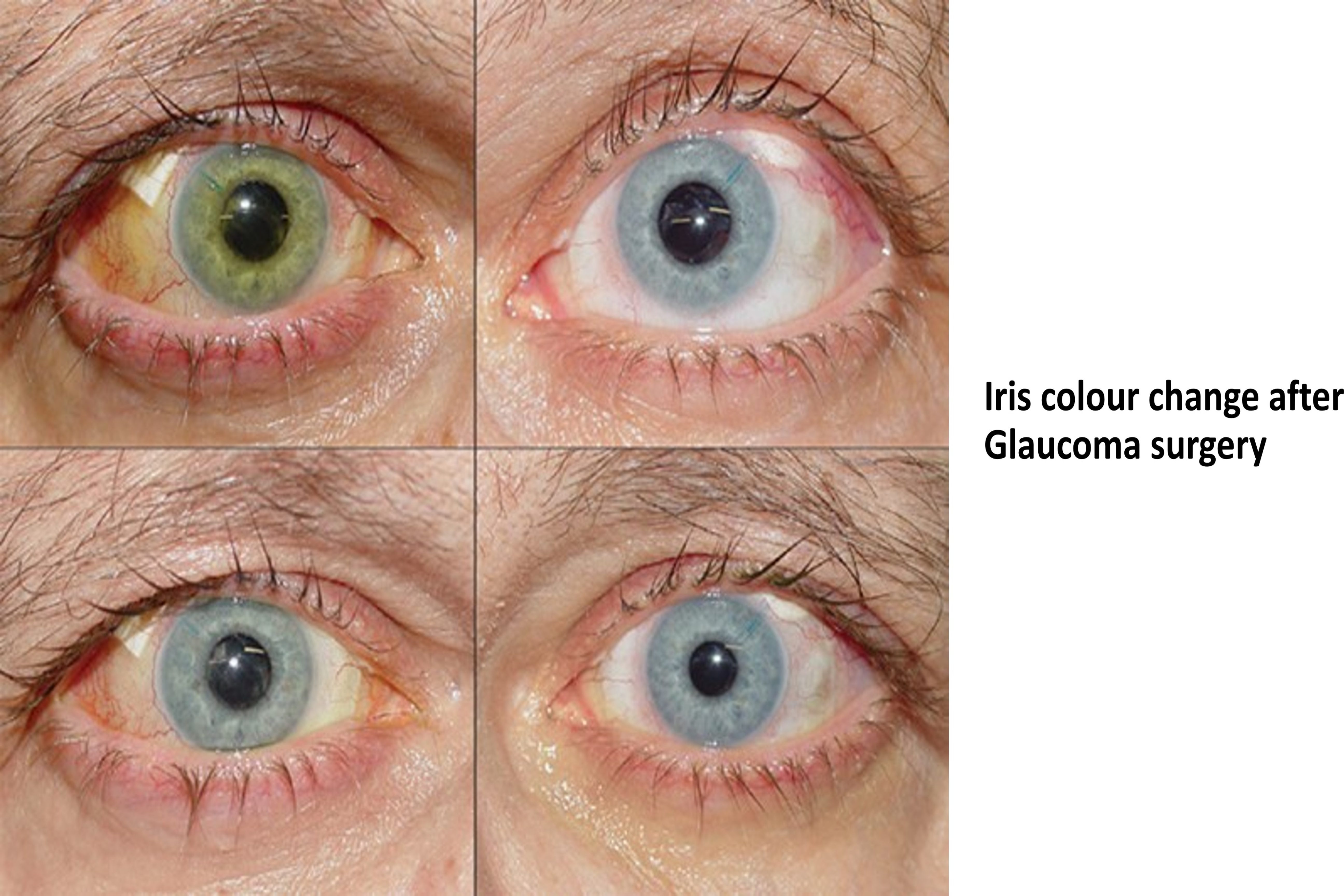
- Eye surgery : Certain types of eye surgery, such as cataract surgery, can lead to secondary glaucoma as a complication. This can occur due to damage to the eye's drainage system during surgery or as a result of inflammation following the procedure.
- Vascular disorders : Diseases affecting blood vessels in the eye, such as diabetic retinopathy or central retinal vein occlusion, can sometimes lead to secondary glaucoma due to impaired blood flow and subsequent damage to the optic nerve.
- Congenital abnormalities : Some babies are born with abnormalities in the eye's drainage structures, predisposing them to develop glaucoma at a young age. This is known as congenital glaucoma, which is a type of secondary glaucoma.
Management of secondary glaucoma involves treating the underlying cause while also addressing the elevated intraocular pressure to prevent further damage to the optic nerve. Treatment may include medications, laser therapy, or surgical interventions such as trabeculectomy or drainage implant surgery, depending on the severity and cause of the glaucoma. Regular monitoring by an ophthalmologist is essential to manage secondary glaucoma effectively and preserve vision.
Symptoms of glaucoma may not be noticeable in the early stages, but as the condition progresses, it can lead to peripheral vision loss and eventually blindness if left untreated. For glaucoma therapy and early detection, routine eye examinations are crucial. Treatment options include prescription eye drops, oral medications, laser therapy, or surgery to lower eye pressure and prevent further vision loss.
Glaucoma screening and surgical solutions:
Glaucoma is a group of eye conditions that damage the optic nerve, usually due to increased pressure within the eye. Screening for glaucoma typically involves a combination of comprehensive eye exams, tonometry (measuring intraocular pressure), visual field testing, and optic nerve imaging. Early detection is crucial to prevent vision loss, as glaucoma often progresses without noticeable symptoms until significant damage has occurred.
Screening for glaucoma is recommended for individuals at higher risk, including those over 40, individuals with a family history of glaucoma, people with diabetes, and those of African or Hispanic descent. However, routine eye exams are essential for everyone, as they can help detect glaucoma and other eye conditions in their early stages.
When it comes to surgical solutions for glaucoma, there are several options available, depending on the severity and progression of the disease:
- Medication : Initially, glaucoma is often managed with prescription eye drops to reduce intraocular pressure. These drops either decrease fluid production in the eye or improve its drainage.
- Laser Therapy : Laser treatments such as selective laser trabeculoplasty (SLT) and laser peripheral iridotomy (LPI) can help improve drainage of fluid from the eye, thereby reducing intraocular pressure.
- Minimally Invasive Glaucoma Surgery (MIGS) : MIGS procedures are relatively new and less invasive compared to traditional glaucoma surgeries. They aim to reduce intraocular pressure by improving the eye's natural drainage system. Examples include trabecular micro bypass stents and minimally invasive glaucoma drainage devices.
- Conventional Glaucoma Surgery : In cases where medication and less invasive procedures are insufficient, traditional glaucoma surgeries like trabeculectomy, or tube shunt surgery may be recommended. These procedures involve creating new drainage pathways for aqueous humor to reduce intraocular pressure.
- Cyclophotocoagulation : This procedure uses laser therapy to decrease fluid production in the eye, thereby lowering intraocular pressure.
The choice of surgical solution depends on factors such as the patient's overall health, the severity of glaucoma, and the presence of other eye conditions. It's essential for individuals diagnosed with glaucoma to work closely with their ophthalmologist to determine the most appropriate treatment plan for their specific needs. Regular follow-up appointments are crucial to monitor the progression of the disease and adjust treatment as needed.
- Cataract Surgery & Treatment
- Multifocal Intraocular Lens (IOL)
- ICL (Implantable Collamer Lens)
- Glaucoma Surgery & Treatment
- Eye Trauma Care
- Oculoplastic, Squint, Ptosis
- Computerized Eye Testing
- Contact Lens Clinic
- Lasik Surgery
- Refractive Surgical Corrections
- Diabetic Retinopathy Screening & Treatment
- Retinal Surgery / Laser Treatment
